Advertisement
Stem cells are body cells capable of differentiating into various cell types—from skin cells to brain cells. Using stem cells taken from the patient themself grants them tremendous medical potential, from reshaping the immune system to producing tissues on demand.
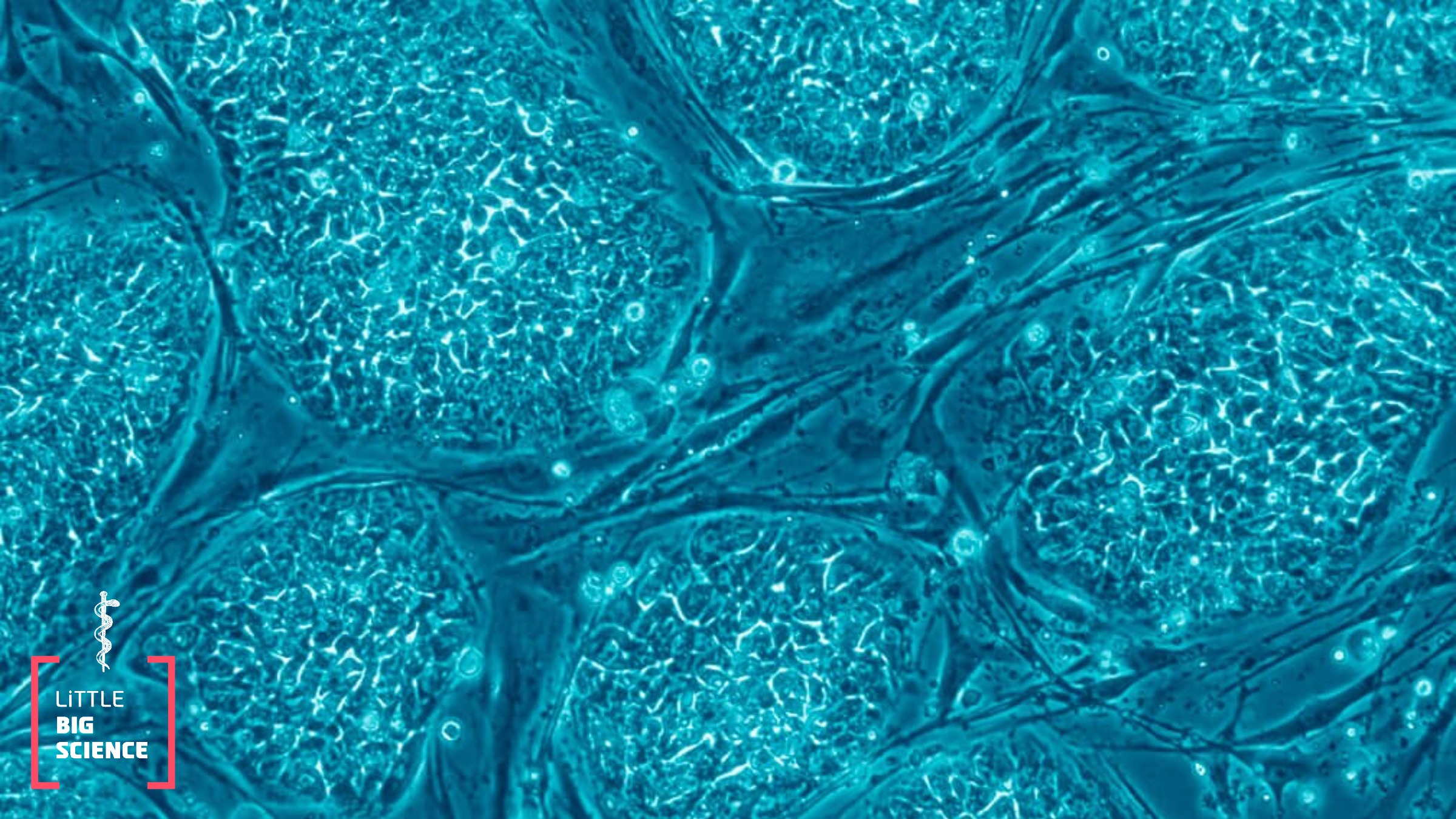
Whether white or Black, women or men, we all begin life the same way: an egg fertilized by a sperm cell starts to duplicate and divide into daughter cells carrying identical genetic material. Later, these daughter cells differentiate into distinct roles—some become nerve cells, others intestinal cells, and so on. Once a cell has differentiated, it usually does not “go back” and cannot adopt other roles. Yet alongside the differentiated cells in our body, there exists a special population of cells that does not fully differentiate but instead remains “master cells,” or “general cells,” whose task is to preserve the body’s capacity to produce different cell types. These are the stem cells, so-called because they can branch into different “offshoots” with distinct functions. When a stem cell divides into two daughter cells, one will differentiate while the other will remain a stem cell, thereby preserving its differentiation potential.
Stem cells themselves differ in the range of cell types they can produce. Stem cells that can give rise to every cell type in the body are called embryonic stem cells, and as far as we know they do not exist in an adult human. Most of the stem cells that remain after birth have partially differentiated and become tissue-specific stem cells. What does that mean? Take the hematopoietic system, for example: in our bone marrow there are stem cells capable of generating all blood cell types—every kind of white blood cell, as well as red blood cells and the cells that form platelets. In other words, these stem cells can give rise to every blood cell, but they cannot produce muscle or lung cells.
It is easy to see why stem cells fascinate the scientific world. In type 1 diabetes (juvenile diabetes), immune cells attack the insulin-producing cells of the pancreas. What could be better than taking the patient’s own stem cells and growing a new pancreas for them? The genetic match would be perfect, and the immune system would not reject the new organ. Unfortunately, we have not yet learned how to grow a complex organ like a whole pancreas in the lab, but it is not inconceivable that we will know how to do it in the coming decades. Currently, this is possible for simpler tissues such as bone marrow, where a treatment that uses stem cells targets blood cancer. Cancer occurs when a differentiated cell acquires a series of mutations that transform it into a cancer cell. In certain types of blood cancer, therapy involves destroying the patient’s bone marrow and transplanting a new one. Because the cancerous mutations occurred in a differentiated cell rather than in stem cells, there are cases in which the new marrow does not come from a donor but from the patient’s own stem cells, harvested before destruction and reintroduced to generate healthy tissue. Similarly, experimental treatments now aim to replace the immune cells of type 1 diabetes patients with stem-cell-derived cells, hoping they will not attack the pancreas and thus will halt the disease.
Stem-cell therapies are also being developed for neurological diseases such as ALS and multiple sclerosis. Multiple sclerosis is an autoimmune neurological disease in which immune cells attack the fatty sheath of nerve cells in the brain and spinal cord, causing irreversible damage to nervous-system function. In an innovative therapy, patients’ immune cells are replaced with new ones derived from stem cells, in the hope that these new cells will not attack the nerve-cell sheath. In contrast, ALS—also known as Lou Gehrig’s disease—is a degenerative muscle disease in which motor neurons die. Several companies (including the Israeli firm BrainStorm) are currently developing an experimental treatment in which stem cells are grown from a patient’s own cells and the resulting material is used in therapy. The hope is that this will keep motor neurons alive.
So far we have seen the therapeutic potential of stem cells for many diseases and stem cell based treatments are under way at various stages of clinical trials. So why are there so few approved treatments?
Despite their great promise, stem-cell research is still in its infancy. One of the most significant challenges is learning how to coax stem cells to differentiate into the desired cell type, something we can currently do only partially. The better we understand the mechanisms that govern cell differentiation, the better we will understand how stem cells operate — and how to guide them to become the cells needed to develop treatments for countless diseases.
English editor: Gloria Volohonsky
Further reading:







