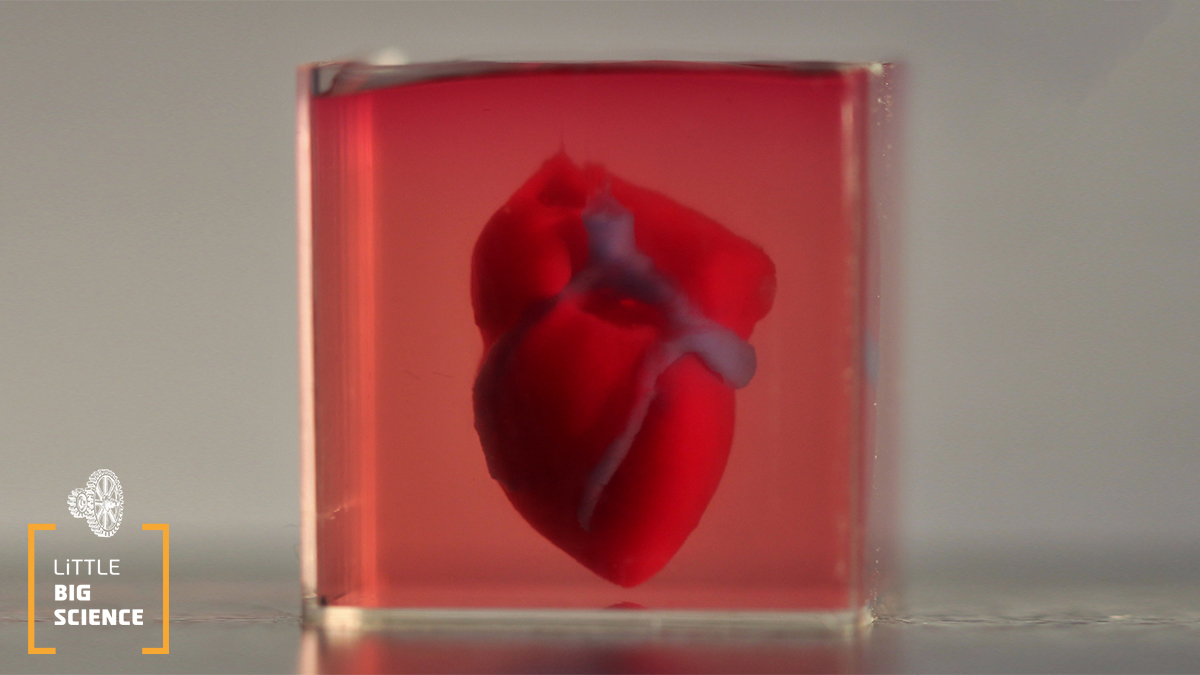
Researchers from Tel Aviv University have successfully printed a small, living heart tailored to the personal characteristics of patients [1]. They created several kinds of bio-ink required to generate the range of cells essential for building the heart and used a biological 3-D printer to print a miniaturized heart. Printing organs in this way could in the future allow faster and safer transplants, as patients who receive them would not need anti-rejection drugs.
Advertisement
Organ transplantation is an extremely complex process. Since organs can not be simply exchanged between people, patients in need of a transplant must wait for a matching donor. Criteria for a match include blood type, body size, compatibility of immune system proteins and other parameters. Even if a suitable donor is found, the waiting period is long and exhausting. Sometimes this problem persists even after the desired donor is found. Patients must take anti-rejection drugs for a long time after the complex transplant surgery, which leaves them vulnerable to infections and diseases. Even after a successful transplant with no rejection for an extended period, many recipients still do not regain full functionality. The surgery often only grants them a few additional months or years in better condition [2].
At first glance, it seems that we solved this problem years ago. We know how to clone animals, so why can't we clone organs? We could take a sample of the patient’s own cells, transform them into heart cells, and grow a new, living heart in the laboratory. This heart would be a healthy “copy” of the patient’s original, diseased heart. However, it is not that simple. Cells grown in the laboratory require a support system to guide them to their correct position and function in the new organ. The individual heart cells need "scaffolds" on which they can organize, and without these scaffolds the cells grow into an uneven, unsynchronized mass. Without support, each cell beats at its own rhythm, instead of performing the synchronized contractions of a healthy heart.
“No problem. We’ll build the scaffolds.” These scaffolds must be made of a material that cells can recognize and can bind to. Most importantly, they must not harm the patient’s body. The body creates its own “scaffolds” from connective tissue based on collagen protein fibers. However, collagen does not have a long shelf life and cannot be stored for later use. In addition, the new heart must be connected to the body’s intricate vascular system. For the new heart to integrate well, it must fit perfectly, considering that each patient has a slightly different body structure.
In Prof. Tal Dvir’s lab at Tel Aviv University, they took the “personalized heart” concept to the next level. In a single step, they would 3D-print both the required scaffolds and the cells that can “decide” which cell type they will become, resulting in a complete heart emerging from the printer. This ambitious plan required teamwork. Biologically, they needed a way to revert adult human cells to a stem cell state. Cells in this state can then become into any cell type in the body [3]. Then, they had to direct these stem cells to differentiate into specific heart tissue cells. From the materials engineering perspective, they had to find a way to use the body’s own building blocks to create an “ink” suitable for printing. The ink they developed is based on collagen fibers from abdominal fat tissue. This mixture forms a thin, weak gel at room temperature (a post on “what is a gel” is coming soon) and hardens and strengthens at 37 °C (body temperature). From this basic ink, they prepared two more specific inks: one containing cardiac muscle cells and one containing vascular (blood vessels) cells.
Next, they needed a 3D printing design. To create it, the researchers used 3D drawings of the heart they wanted to replicate. These drawings were based on data from computerized tomography (CT scans) However, imaging alone was not enough because CT scans lack the resolution to model all the fine capillaries that form the vascular network. Therefore, the researchers had to simulate the vascular network and add it to the design.
Now that they have the ink and the design, can they 3D-print a heart? In theory, yes. However, the printed heart would collapse under its own weight before the printing process is complete. A common practice in 3-D printing design is to include temporary supports to bear the weight of the printed object until printing is finished. Once printing is complete, the final configuration is already stable enough, but there must be a way to remove the supports without damaging the 3D-printed heart. Therefore, the final stage of the printing project was to develop a material that would support the forming heart and could be safely removed from the finished organ. In this case, the material is a variation of the substance commonly used in Petri dishes, and it also has a jelly-like texture.
We can now 3D-print hearts on demand. However, we are just getting started. The miniature heart that the researchers printed had the complex anatomical structures necessary for a living heart and demonstrated mechanical stability. The researchers emphasize, however, that one more critical step is necessary before this technology can be used on patients: post-printing processing. This processing must include cultivating the printed organ with access to oxygen, nutrients, electrical signals, and biochemical signals. This will allow the organ to “mature” and prepares it for transplantation. We will also need to ensure that the mature organ does not trigger an immune response in the patient. Once we figure out how to accomplish this, we will be closer to the day when we can print organs for transplantation in clinical settings. With the publication of this research, that day seems closer than ever.
English editing: Gloria Volohonsky
Sources:
[1] The original article published in the journal “Advanced Science”
[2] A review of the four most common types of organ-transplant surgeries
[3] “Stem cells – because the body has spare parts?”








