A research team from Zurich has developed a system intended to serve as an alternative to antibiotics and to confront one of the most stubborn and antibiotic-resistant infectious agents—Staphylococcus aureus. The system is based on engineered cells designed to detect the bacterium in our bodies and destroy it.
Advertisement
Healthcare-Associated Infections (HAIs) are one of the key challenges faced by modern medicine today. In the United States, about 700,000 people a year contract such infections, of whom roughly 70,000 die [1]. One of the leading infectious agents in hospitals is the bacterium Staphylococcus aureus, which causes a wide range of symptoms and complications—from superficial skin infections to life-threatening conditions such as pneumonia, meningitis, and sepsis [2].
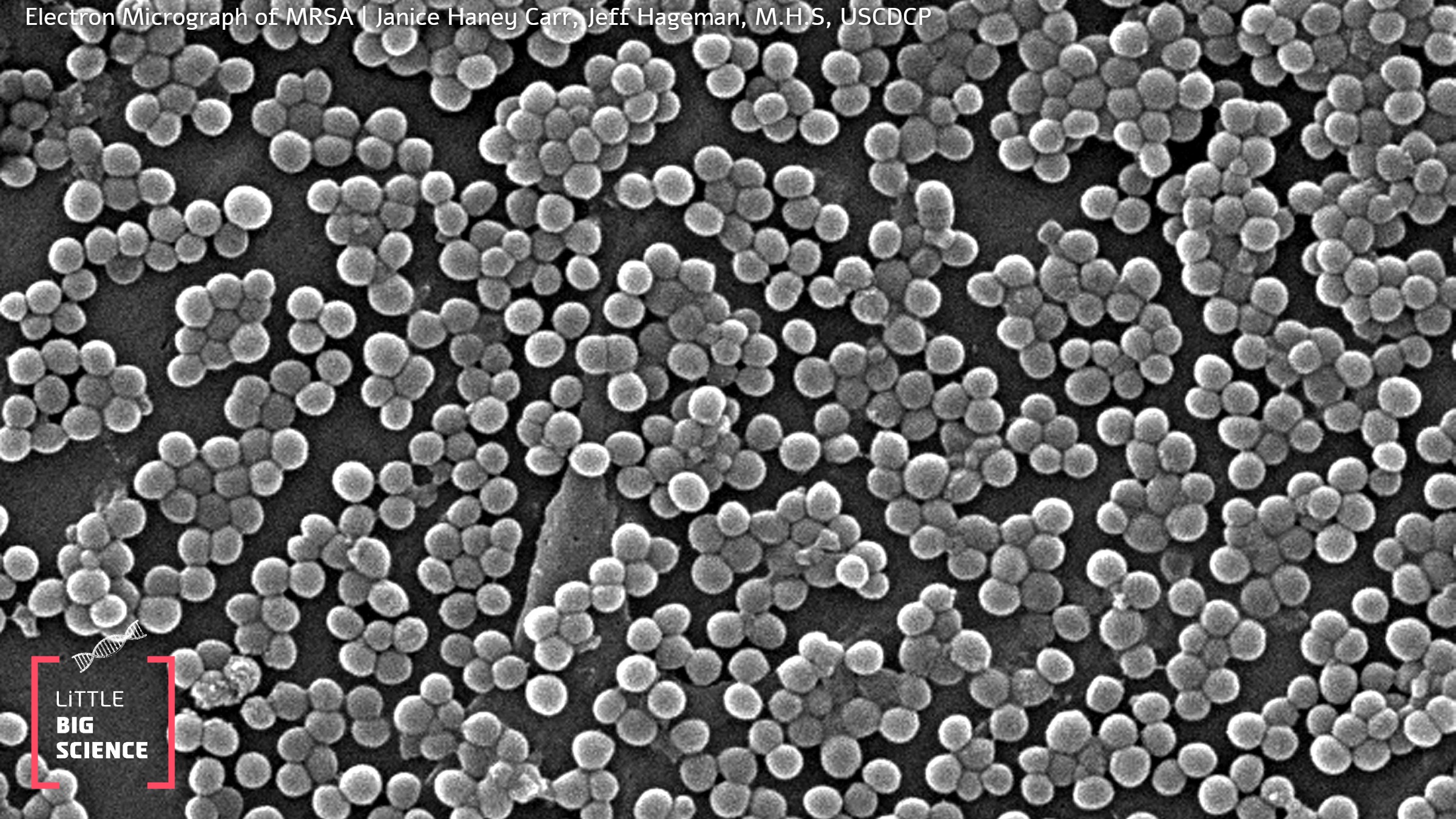
Two principal factors make this bacterium such a successful disease-causing agent. The first is its ability to form a membrane composed of numerous S. aureus cells together with secreted substances, known as a biofilm. The biofilm tends to form on many surfaces—from medical devices to various tissues and implants in the human body. Bacteria embedded in this structure are hidden from their surroundings and therefore tend to be less susceptible to the immune response and to antibiotics [3]. The second factor is the species’ propensity to develop resistance to a broad spectrum of antibiotics. Methicillin-resistant Staphylococcus aureus, or MRSA, is one of the most challenging resistant strains to treat.
Our immune cells can recognize the bacterium via dedicated receptors called Toll-like receptors (TLRs), which detect molecules located on the bacterial surface [4]. This recognition triggers the secretion of proteins called chemokines that "call in" additional immune cells to reach the site. Nevertheless, S. aureus has evolved many mechanisms that help it evade our immune system [5]. In a 2018 article published in the prestigious journal Cell, researchers from ETH Zurich decided to harness these receptors and engineer a human-cell-based system that can efficiently detect the bacterium’s presence and respond directly and immediately [6].
The researchers engineered human embryonic kidney cells to recognize the bacterium through TLRs. In this design, instead of secreting proteins that recruit immune cells, the cells secrete a protein that immediately kills the bacterium in close proximity to them. For this task the researchers selected the enzyme lysostaphin, originally derived from a “cousin” of this bacterium, another staphylococcal species—Staphylococcus simulans. This enzyme destroys the cell wall of S. aureus, leading to bacterial death [7]. Preliminary in vitro experiments showed that these engineered cells can indeed detect and eradicate S. aureus, including MRSA strains.
Next, in preparation for testing in mice, the researchers faced the challenge of introducing the system into a living body without provoking the host immune response. They encapsulated the engineered cells in microscopic capsules with tiny pores that allow the cells to sense the bacterium yet block entry of the larger immune cells. Because one common complication of the bacterium is biofilm formation on biomedical implants, the researchers used mice with dummy implants as a model. To evaluate the system’s preventive potential, they injected the encapsulated engineered cells into mice before infecting them with MRSA. The results were striking: in 10 of 11 mice no bacterial presence was detected and no biofilm formed on the implants, whereas all control-group mice developed an infection. To test the system’s therapeutic capability, a second experiment injected the engineered cells after MRSA infection. All eight treated mice recovered completely, compared with 3 of 8 mice treated with vancomycin, the current standard antibiotic used for MRSA infections [8].
Although such a precisely targeted system appears to be an ideal solution, many challenges remain before it can be approved for human use. These include assessing the long-term stability of the cells and capsules, developing methods to deactivate the system if necessary, and of course thoroughly examining potential side effects. One possible side effect of a proliferative cell-based therapy is the formation of malignant tumors [9]. Nonetheless, the researchers are optimistic and believe that such a system could offer an alternative to antibiotics in an era of mounting bacterial resistance.
English editing: Elee Shimshoni
References:
- Centers for Disease Control and Prevention (CDC) data on hospital-acquired infections
- Review of Staphylococcus aureus infections
- Review of S. aureus biofilms
- Review of the innate immune response to S. aureus
- Review of S. aureus cell wall proteins
- The study describing the system—Immunomimetic Designer Cells Protect Mice from MRSA Infection
- Article on the efficacy of lysostaphin against S. aureus
- Clinical practice guidelines for the treatment of MRSA infections by the Infectious Diseases Society of America
- Study demonstrating the tumorigenic potential of human embryonic kidney cells in immunocompromised mice







