
An outbreak of tuberculosis in Rehovot has (again) made headlines about one of the world’s most common infectious diseases, which kills about one and a half million people each year, and whose causative bacteria are becoming resistant to antibiotics.
Advertisement
In February 2025, 11 children and two preschool teachers in Rehovot contracted tuberculosis [1]. The source of the outbreak was one of the teachers. All patients received antibiotic therapy and are expected to recover. The prevailing assessment is that the teacher was a carrier of the tuberculosis bacterium, which she probably contracted in childhood, and that the disease was recently reactivated.
Each year, nine to ten million new patients are diagnosed worldwide, most of them in developing countries, and about one sixth of them—roughly 1.5 million people—die of the disease. Two main factors drive this high mortality: infection in HIV carriers, who are more vulnerable than the general population, and the evolution of bacterial strains that cause tuberculosis and are resistant to most existing drugs.
Tuberculosis [2, 3] has accompanied humans for at least 10,000 years. The earliest evidence appears in Neolithic skeletons and mummified remains from Egypt. A similar disease exists in cattle, and it is thought that the pathogen “jumped” to humans following cattle domestication for milk production. As long as humans lived in small groups, outbreaks were local and the disease was not a major problem. The increase in population density that followed the Industrial Revolution and urbanization enabled tuberculosis to spread, and in the 17th and 18th centuries one in four people in the Western world died from it. Even today, those at the highest risk of infection are people residing within crowded indoor settings—detention centers, prisons, homeless shelters—and educational institutions.
Tuberculosis can manifest in various parts of the body: lungs, bones, nervous system, and skin. Only in the mid-19th century was it recognized that these were different manifestations of a single disease. In 1882 Robert Koch identified the bacteria causing the illness. He succeeded in culturing them in the laboratory (a colony develops in about two weeks) and proved that they are the causative agents. For this discovery he received the 1905 Nobel Prize in Medicine. The bacteria, called Mycobacterium tuberculosis, are aerobic rod-shaped bacteria with an exceptionally rigid cell wall that is impermeable to standard bacterial stains.
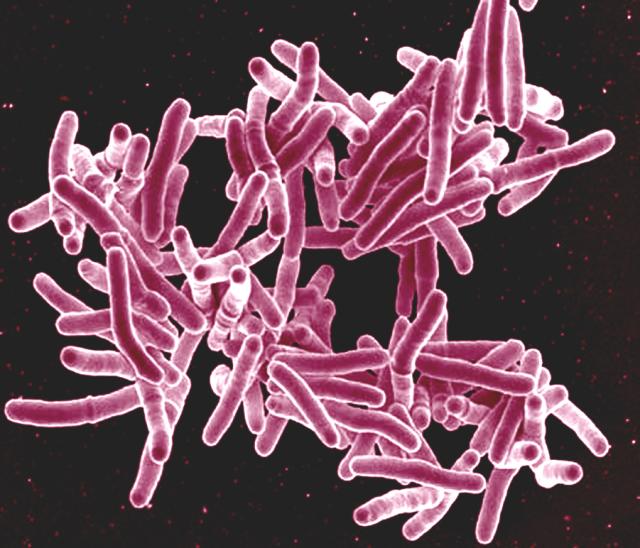
Scanning electron micrograph of Mycobacterium tuberculosis bacteria. Source: NIAID via Wikimedia Commons
Tuberculosis is transmitted via the respiratory tract. A single bacterium entering the airways is sufficient to infect a person, yet only 5 %–15 % of those exposed will develop an active disease. The bacteria reach the lungs and create inflammatory foci. White blood cells, mainly macrophages, which are cells that engulf pathogens and destroy them in an intracellular structure called a lysosome, gather around these foci. Antibodies against the bacteria help macrophages engulf them, but instead of being destroyed, the bacteria block entry to the lysosome and replicate inside the macrophages. In children this stage may pass without symptoms.
If the foci do not heal, the bacteria continue to multiply within the macrophages that accumulate at the center, forming a granuloma. A granuloma is a structure generated by macrophage aggregation around a substance the immune system perceives as foreign; its role is to sequester and contain the threat when it cannot be eliminated. Cells in the center die from lack of oxygen, producing necrosis from which bacteria erupt into the bloodstream and disseminate to other tissues.
If the focus heals, as happens in most children, latent bacteria remain inside the macrophages. They may persist for decades, and the disease can reactivate in old age when the immune system weakens. It is estimated that one-third of the world’s population carries the bacterium in this latent state. The disease can be treated with various antibiotics, usually a combination of two or more, unless the bacteria are already resistant to them.
Data from the Ministry of Health show that in Israel roughly 200 cases per year were reported between 2021–2024 [4]. Carriers exist in Israel as well, but no information or estimates are available on their number. Latent tuberculosis can be detected by a blood test or a skin test, for detecting an immune response to the bacterium. However, a non-carrier who was previously vaccinated with the BCG vaccine may test positive.
The BCG vaccine, developed in 1921 by Albert Calmette and Camille Guérin, was based on Mycobacterium bovis, which causes tuberculosis in cattle and humans. The bacteria were attenuated over 13 years in 230 sequential passages on artificial media. The vaccine did not prevent infection, but it enabled the vaccinated individual to cope more easily with the initial stage of the disease and blocked subsequent stages. Widely used, it helped reduce global case numbers, but the immunity it conferred was short-lived (about ten years). Another drawback was tuberculosis in HIV carriers and AIDS patients. Today this formulation is used only in regions where tuberculosis is common.
Researchers are now seeking a better alternative that provides longer-lasting immunity, thereby helping to eradicate the disease completely and protecting the older population as well. Several vaccine candidates of different types are in various stages of development and clinical trials. When the time comes, we will be happy to report the success of one, or more, of them.
Hebrew editing: Smadar Raban
English editing: Elee Shimshoni
References:
[1] Health Intelligence report – Ministry of Health – March 2025
[2] About tuberculosis – World Health Organization website
[3] About tuberculosis – U.S. Centers for Disease Control and Prevention
[4] Tuberculosis morbidity data in Israel – Ministry of Health







