Advertisement
In the 1950s the structure of DNA was discovered, and with it its significance: DNA is the “recipe book” for producing our proteins—muscle fibers, enzymes, receptors, antibodies, and more. Accordingly, changes in the DNA sequence (mutations) can lead to alterations in the resulting protein. These changes can be destructive and cause disease. For example, a mutation in muscle proteins can cause muscular dystrophy, whereas a mutation in an immune-system receptor can lead to severe immunodeficiency. Genetic research advanced rapidly, as did attempts to develop gene-therapy methods aimed at correcting disease-causing mutations. Yet one major challenge stopped the researchers: how can we deliver the intact DNA segment into cells and make them manufacture functional proteins from it?
The solution chosen was viruses: viruses carry their own genetic material, DNA or RNA, but lack the tools to produce the necessary proteins on their own. Therefore, to reproduce they must inject their genetic material into a host cell that will manufacture it for them. In other words, viruses are experts at introducing DNA fragments into cells and getting them to synthesize proteins—exactly what we needed. Indeed, in the 1980s the first gene-therapy trials using viruses were conducted. Instead of harboring DNA segments for manufacturing viral proteins, scientists engineered the viruses to carry segments for manufacturing normal human proteins and inserted them into human DNA. In the 1990s, several children were treated this way, but a few years later it became clear that the celebration was premature: some of the children developed cancer following the therapy. Tests showed that the cancer was caused by the treatment itself, because when the engineered virus inserted the corrected segment into the patients’ DNA it disrupted other essential genes. These severe outcomes almost completely halted gene-therapy efforts. Such cases cannot be ruled out, since we cannot control the location where the virus inserts the engineered DNA fragment.
Nonetheless, a few years ago, CRISPR burst into our lives: no more random insertion of DNA segments! CRISPR is a sophisticated genetic-engineering method that overcomes the problem of viral random insertion. Its advantage lies in its ability to choose the DNA insertion site with precision. So why is CRISPR not yet used for gene therapy? CRISPR is based on a natural bacterial defense system and requires a bacterial enzyme to function. To use CRISPR in human cells, that bacterial enzyme must be delivered into them. This brings us back to the starting point: how do we introduce a whole enzyme or a DNA segment that can make such an enzyme into human cells? So far, studies have used viruses to deliver the enzyme-coding segment—an approach that, as noted, can be problematic, and substantial efforts are underway to overcome this hurdle. One solution is to use viruses that do not integrate their DNA into ours but limit themselves to a temporary infection of the cells. This, too, can be problematic, because our cells can detect a viral infection, mount a response against it, and degrade its genetic material—possibly before the enzyme is even produced. Moreover, in some cases an infected cell will destroy itself in a controlled process (apoptosis) to prevent the virus from spreading to neighboring cells.
We therefore need a method that does not require viruses at all. That is precisely what researchers at the University of California, San Francisco accomplished in a study published in the prestigious journal Nature. They tested thousands of experimental conditions until they found an alternative approach that allows CRISPR to be used without any dependence on viruses. Their method involves treating cells with a gentle electric current, temporarily creating tiny holes in the cell membranes that allow DNA fragments from the surroundings to enter. In this way they succeeded in correcting mutations in cells from patients with genetic diseases. At this stage, the repaired cells have not been transplanted back into the patients, so it is not yet certain that these individuals will fully recover. Nevertheless, the research team managed to use their method to cure mice carrying mutations analogous to those found in humans.
The next step is to see whether the same method can be applied in humans and whether unexpected side effects emerge. If it succeeds as expected, this approach will represent a significant breakthrough in gene therapy. It could even improve existing treatments, such as engineering immune cells to attack cancer (CAR-T).
English editing: Elee Shimshoni
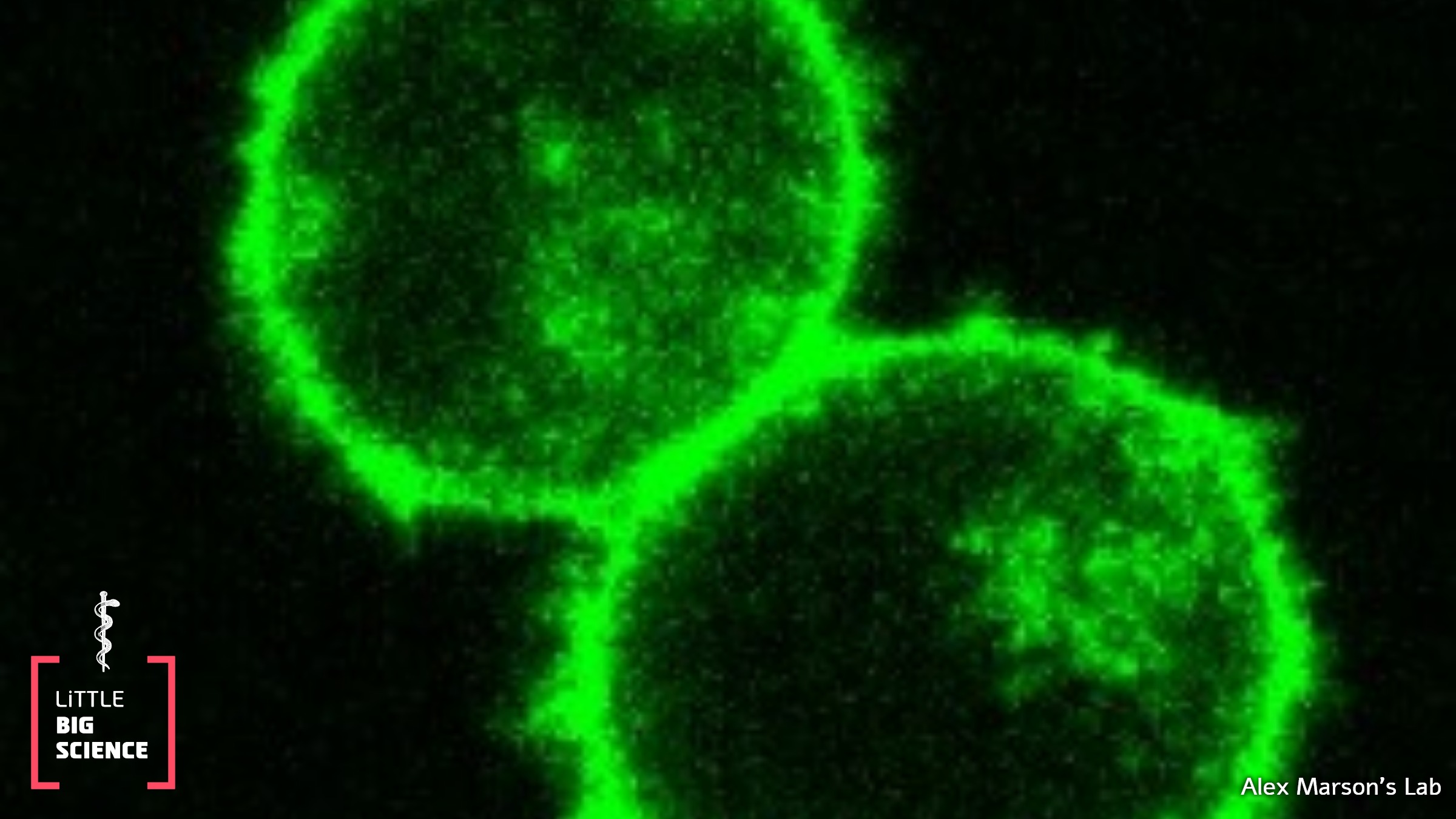
Main image: Alex Marson’s Lab
In the image: engineered cells created by the researchers to test the new system







